Harvard Business Review occasionally brings into focus the issues that plague health care systems, particularly the US system. The recent three months of issues have all had interesting commentaries:
In September, a lengthy piece by Robert Kaplan and Michael Porter posits that the burgeoning costs of healthcare can be better managed and controlled through a form of activity-based costing – detailed process mapping to track the costs of delivering care at the individual patient level (rather than at the level of the ‘average patient’ with for example a knee replacement with risk adjustments etc). Another highly regarded HBS Professor, Regina Herzlinger, follows up in October with a letter rebutting this thesis by pointing out that the model denies the reality of extreme patient-to-patient variability and that it will simply be too complex to mount the effort required to analyze the complexity inherent in such variance, especially with comorbidities. The interchange goes on with a further response by Kaplan and Porter which reemphasizes central tenets of the original piece (e.g. tracking of costs not charges to insurance or patients) and that their approach should result in being able to line up costs against outcomes to enable informed decisions about contracting and reimbursements.
In November 2011, McGill University’s Professor Henry Mintzberg comes at healthcare fixes with a different lens – we should adopt successful practices in healthcare delivery that are already shown to work. He cites several examples:
- Use of internal clinicians to craft and implement real improvements, not the ideas or recommendations from external experts;
- Establish and nurture professional communities that engage those at the front line of care rather than having those doctors and nurses sit powerless and stifled in a controlled hierarchy;
- Stop advocating that a privately governed health healthcare system is better than a publically controlled one – the argument is irrelevant since at its core most health systems involve both private and public entities and activities;
- Encourage greater collaboration in a system-wide approach rather than the focus being upon a single episode of care.
The first three authors from HBS grapple with how to drive costs down from above with some form of connecting the dots of costs, charges and outcomes whereas the last author sees solutions coming from within the system, empowering the front line providers to implement (and presumably adapt) known solutions.
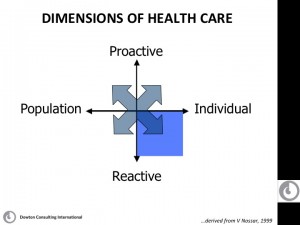
These ideas all contribute value to the ongoing debate. All explicitly or obliquely acknowledge that costs and healthcare solutions are heavily influenced by physician behaviors and the drivers of their professional behaviors. Without dedicated focus to engaging physicians and their professional organizations in both understanding and owning the issues of healthcare in detail, it seems little will be achieved. Medical education must address this reality at every level (medical student, residency, fellowship and continuing medical education). At the moment, medical education focuses heavily on the lower right quadrant of the attached diagram – until we seriously move the balance of medical education to be more encompassing of the other quadrants and / or adjust the drivers of physician reward to play outside individual acute patient care, it seems that any of these proposed solutions can help but will not be enough for sustainability.